Legionella cases on the rise
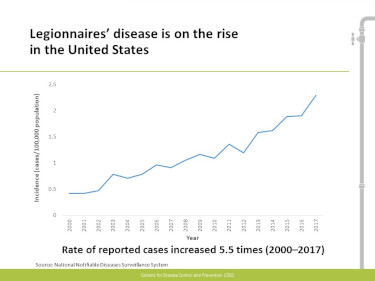
The Centers for Disease Control and Prevention reported that from 2000 to 2017, the number of confirmed cases increased more than fivefold, but notes the number may be much larger because legionellosis is often missed as a diagnosis.
Legionellosis is caused by the Legionella bacteria, which occurs naturally in lakes and streams, and other fresh water environments. Legionella can become a public health concern when it spreads to a building’s plumbing system and then through hot water tanks, shower heads, faucets, fountains and other equipment connected to the contaminated plumbing system.
Legionellosis is spread through water droplets small enough to breathe. A less common exposure may happen when people drink contaminated beverages that accidently go to the lungs when they swallow.
Most healthy people exposed to Legionella do not get sick. People who are at greater risk of contracting the illness are those who are more than 50 years old; former or current smokers; and patients with chronic lung diseases, cancer or other underlying illnesses. Officials from local public health departments and the Iowa Department of Public Health (IDPH) work together to interview people with reported legionellosis to identify possible shared exposure locations and other risk factors.
Although no single reason has been identified, the spike could be due to a variety of factors including greater awareness of legionellosis and, therefore, more testing; an increase of Legionella in the environment; greater patient susceptibility; or some combination of these.
In 2018, a State Hygienic Laboratory team led by the Office of Research and Development Director Lucy DesJardin developed a project using next generation sequencing for whole genome sequencing analysis of Legionella bacterial species isolated from premise plumbing systems of hospitals in the Midwest. Results showed that Legionella pneumophila samples were genetically conserved over time and location in plumbing systems, and provided guidance on what type of water sampling plan would be best in the event of investigating the source of a Legionella outbreak.
Legionella samples were also examined for antibiotic resistance genes and virulence factors as a measure of pathogenicity and to guide what type of remediation would be best for the strain of bacteria found. These studies are being expanded to include metagenomics analyses (the study of genetic material) of water from plumbing systems that receive different types of decontamination treatments.
Testing informationThe recommended tests for diagnosing legionellosis include both a culture of a lower respiratory specimen on selective media and the Legionella urine antigen test. While the urine antigen test can produce a quick result, it can only detect Legionella pneumophila serogroup 1. A patient with a negative urinary antigen test may have Legionnaires’ disease caused by other Legionella species or serogroups.
A lower respiratory specimen culture can detect multiple species and serogroups and allows for comparison of clinical and environmental isolates to identify possible sources of infection. Specimens sent to SHL for Legionella culture can also be tested via PCR, which has a quicker turnaround time than culture. SHL can perform Legionella cultures from both clinical specimens and environmental sources. When possible, IDPH encourages health care providers to submit a pre-antibiotic treatment specimen for culture and/or PCR.
For more information, contact SHL at 319-335-4335 or visit the SHL website for test details, and collection and submission instructions, including culture testing with or without PCR or for PCR-only test requests.